Autism Spectrum Disorder (ASD) is a developmental condition that affects a person’s ability to communicate, engage in social interactions, and process sensory information. The frequency of autism is rising globally, with one in 36 children in the United States being diagnosed with the disorder CDC, 2023. Although early diagnosis and intervention have been shown to improve outcomes for children with autism, racial disparities persist in the medical community, particularly for children of color. Children from marginalized racial groups, including Black, Hispanic, and Indigenous children, often experience later diagnoses, limited access to services, and cultural barriers that hinder effective treatment.

Racial disparities in the autism diagnosis and treatment process reflect broader societal issues, including systemic racism, socioeconomic inequality, and cultural misunderstandings. For many families of color, the challenges are compounded by insufficient healthcare access, financial burdens, and cultural barriers that make it harder to seek or receive help. These delays in diagnosis and treatment can have a profound impact on children’s developmental outcomes, affecting their education, social integration, and overall quality of life. By addressing these disparities, we can ensure that children of color with autism have equal opportunities to thrive and succeed.
Real-life experiences shed light on the severity of these disparities. For example, a mother of a Black child with autism shared her story in an interview with the Autism Society. She recounted how her son, who was nonverbal and struggled with social cues, was not diagnosed until the age of five. Despite noticing early signs, she faced dismissive attitudes from healthcare providers who attributed her son’s behavior to “disciplinary issues.” It wasn’t until she advocated relentlessly that her child was diagnosed and provided access to early intervention services. Her experience illustrates how racial biases in healthcare can lead to delayed diagnoses for children of color, ultimately hindering their access to essential services.
Importance to Behavioral Neuroscience and Biopsychology Research
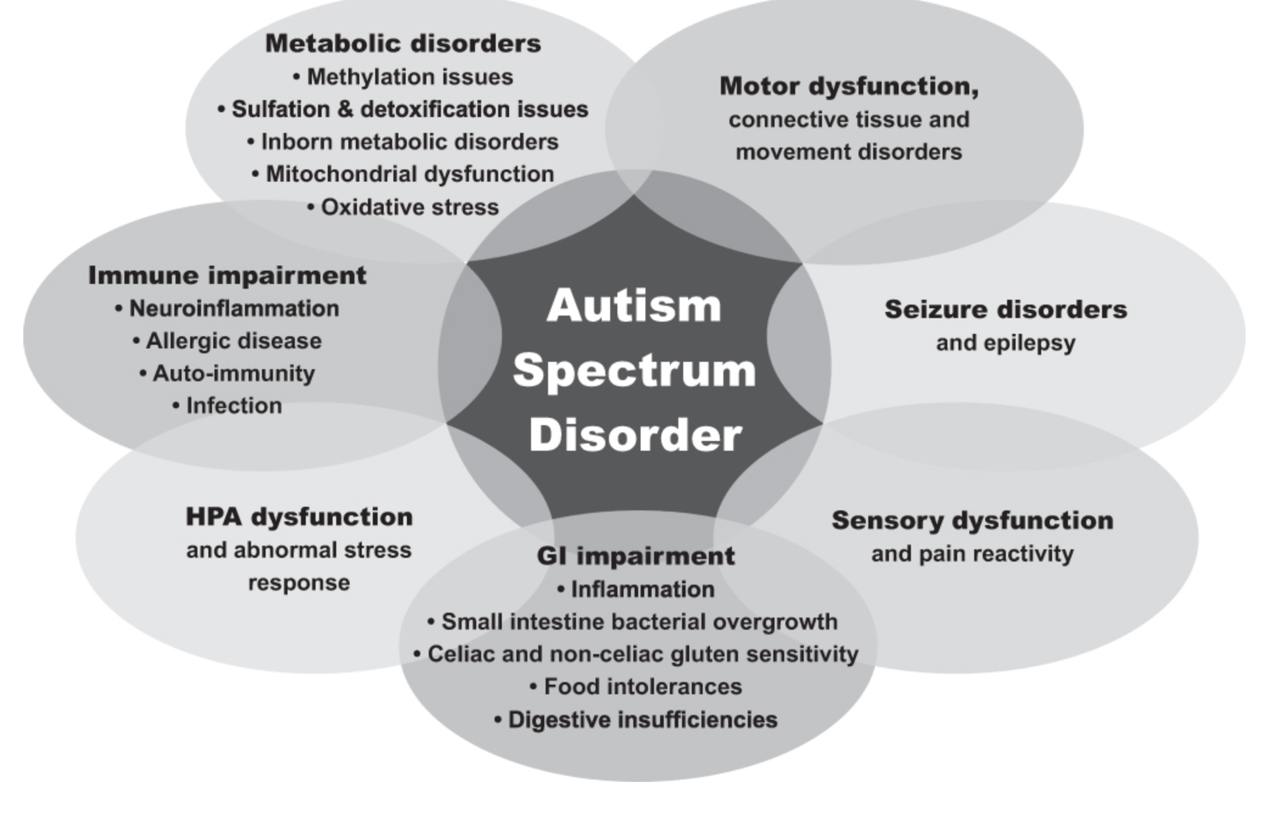
Research in behavioral neuroscience and biopsychology plays a crucial role in understanding the neurological foundation of autism and the impact of early intervention on brain development. Studies have shown that autism is associated with differences in brain structure and function, particularly in areas related to social behavior, communication, and sensory processing (Courchesne et al., 2007). Early diagnosis and intervention, particularly in the first few years of life, can lead to improvements in brain plasticity, enhancing a child’s ability to learn new skills and adapt to their environment (Dawson, 2008).
According to Pinel and Barnes (2001), biopsychology research suggests that early intervention can lead to observable changes in the brain’s structure and function, demonstrating the potential for neuroplasticity in children diagnosed with autism. These findings are significant because they show that interventions that target specific brain functions can improve cognitive and social outcomes for children with autism. However, racial disparities in the diagnosis process can delay access to these beneficial interventions for children of color.
Racial disparities in autism diagnosis also affect the field of biopsychology, the delays in diagnosis prevent children of color from accessing early interventions that could improve cognitive and social development. Biological research on autism continues to evolve, and understanding how early interventions impact brain development is a critical area of study. However, the societal inequalities and cultural factors that contribute to differences in access to these interventions need to be addressed to make sure that research findings are applied fairly to all racial groups.
Theoretical Approaches Driving Research
Several theories shape autism research, especially when looking at racial differences in diagnosis and treatment. These theories focus on different parts of the disorder, like its symptoms and effects, and how it impacts people from various racial and cultural backgrounds. They help researchers better understand how autism might look different in different groups and how to improve care for everyone.
Social Model of Disability
The social model of disability sees disability not as an issue with the individual but as a result of societal barriers that stop people from fully participating in society. This model has influenced autism research by encouraging studies on how social factors, like race and socioeconomic status, contribute to differences in diagnosis and treatment. Research based on this model highlights the need for changes in society’s attitudes and improvements in healthcare systems to help reduce the barriers that children of color face in getting autism services (Oliver, 1996).
Neurodevelopmental Models
These models focus on understanding how autism develops at the level of the brain and the genetic and environmental factors that contribute to its onset. According to Pinel and Barnes (2021), autism is considered a neurodevelopmental disorder in which irregularities in brain development, particularly in areas such as the prefrontal cortex, can lead to the behaviors associated with autism, including difficulties with social interaction, communication, and repetitive behaviors. Research in neurodevelopmental models emphasizes the importance of early intervention to help guide the brain’s development in more adaptive directions.
Cultural Competency in Healthcare
Cultural competency refers to the ability of healthcare providers to understand and address the cultural differences that may affect diagnosis and treatment. In the context of autism, cultural competency is essential for ensuring that children from diverse racial and ethnic backgrounds receive appropriate care. Research based on cultural competency looks at how medical practitioners can be trained to recognize and address the unique needs of families of color, such as offering services in multiple languages or understanding cultural differences in how autism is perceived and expressed. This approach is critical to reducing racial disparities in autism diagnosis and ensuring that all children receive the support they need (Betancourt et al., 2003).
Primary Findings and Examples
Several studies have highlighted key findings related to the racial disparities in autism diagnosis and treatment:
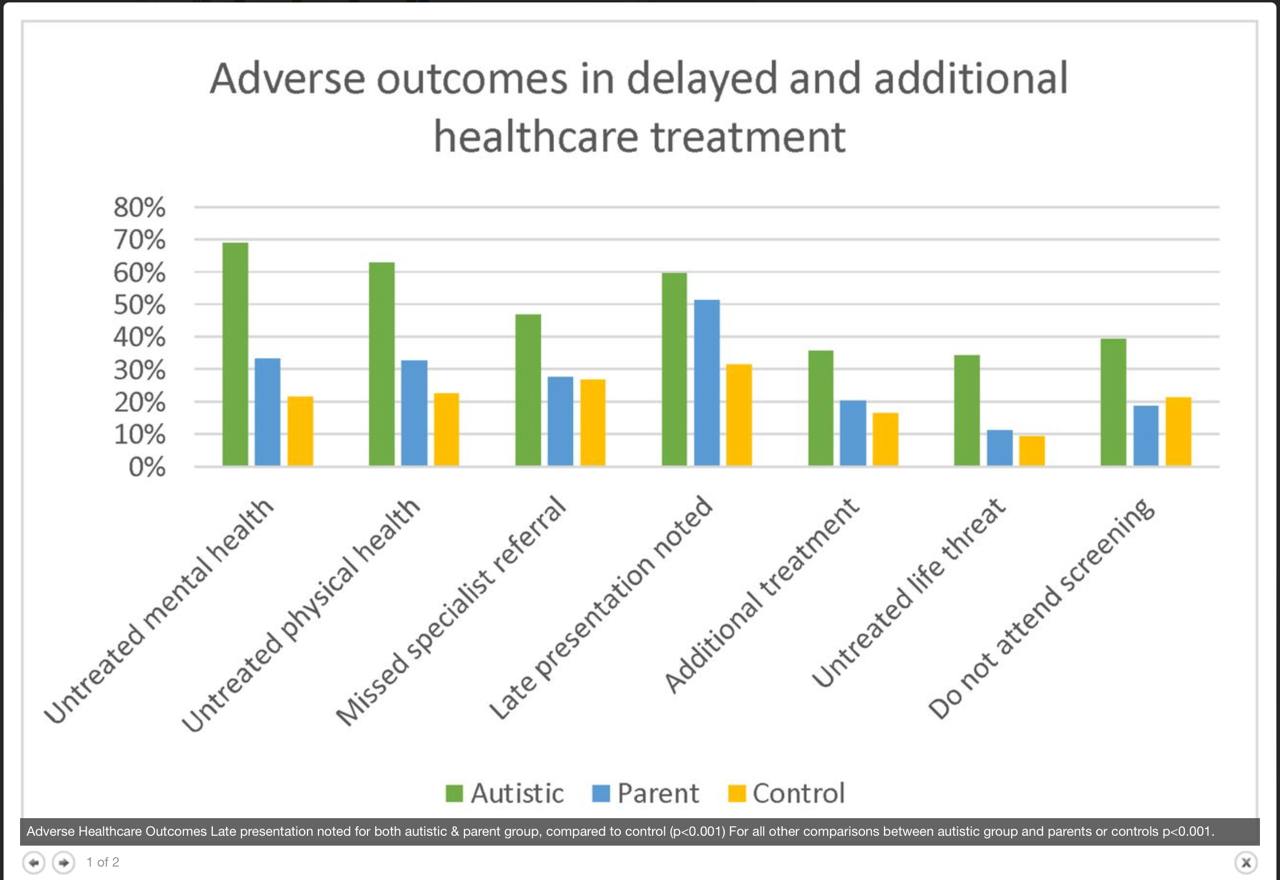
- Late Diagnosis in Children of Color: Research consistently shows that children of color are diagnosed with autism later than their white peers. A study by Zuckerman et al. (2014) found that Black children were diagnosed at an average age of 5.4 years, compared to 3.6 years for white children. Delays in diagnosis often mean that children miss out on critical early intervention services that could improve their developmental outcomes. In many cases, children of color are diagnosed only after their symptoms have become more severe, making treatment more difficult and less effective. (Zuckerman et al., 2014)
- Barriers to Accessing Services: Children of color face multiple barriers to accessing autism services, including financial constraints, lack of insurance, and limited access to culturally competent healthcare providers. A study by Liptak et al. (2008) found that Black children were less likely to receive early intervention services compared to white children, despite having similar levels of autism symptoms. (Liptak et al., 2008)
How Findings Contribute to Understanding the Topic
These findings demonstrate that racial disparities in autism diagnosis and treatment are deeply rooted in both societal and structural factors. By examining these disparities, we can better understand how brain development and early interventions intersect with the experiences of children of color. Research has shown that early diagnosis and treatment are crucial for improving outcomes in children with autism. However, when children of color face delays in diagnosis and treatment, the benefits of early intervention are diminished.
Concluding Remarks and Suggested Avenues for Further Research
To address the racial disparities in autism diagnosis and treatment, future research must focus on several key areas. First, more studies are needed to explore the impact of cultural competence in healthcare settings and how training medical professionals to understand cultural differences can improve outcomes for children of color. Second, researchers should investigate the effectiveness of community-based intervention programs that are tailored to the needs of families from marginalized racial backgrounds. These programs could provide more accessible, culturally relevant services and help bridge the gap in care for underserved communities.
Video and Visual Insights
References
- Betancourt, J. R. (2003). Defining Cultural Competence: A practical framework for addressing Racial/Ethnic disparities in health and health care. Public Health Reports, 118(4), 293–302. https://journals.sagepub.com/doi/abs/10.1093/phr/118.4.293
- Courchesne, E., Pierce, K., Schumann, C. M., Redcay, E., Buckwalter, J. A., Kennedy, D. P., & Morgan, J. (2007). Mapping early brain development in autism. Neuron, 56(2), 399–413. https://doi.org/10.1016/j.neuron.2007.10.016
- Data and statistics on autism spectrum disorder. (2024, May 16). Autism Spectrum Disorder (ASD). https://www.cdc.gov/autism/data-research/index.html
- Dawson, G. (2008). Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology, 20(3), 775–803. https://doi.org/10.1017/s0954579408000370
- Douglas, R. J., & Martin, K. A. (2007). Mapping the Matrix: The Ways of Neocortex. Neuron, 56(2), 226–238. https://doi.org/10.1016/j.neuron.2007.10.017
- Humphrey, N. (2008). Including pupils with autistic spectrum disorders in mainstream schools. Support for Learning, 23(1), 41–47. https://doi.org/10.1111/j.1467-9604.2007.00367.x
- Liptak, G. S., Benzoni, L. B., Mruzek, D. W., Nolan, K. W., Thingvoll, M. A., Wade, C. M., & Fryer, G. E. (2008). Disparities in Diagnosis and Access to Health Services for Children with Autism: Data from the National Survey of Children’s Health. Journal of Developmental & Behavioral Pediatrics, 29(3), 152–160. https://doi.org/10.1097/dbp.0b013e318165c7a0
- Oliver, M. (1996). Understanding disability. https://doi.org/10.1007/978-1-349-24269-6
- Pinel, J. P. J., & Barnes, S. (2021). Biopsychology.
- Zuckerman, K. E., Sinche, B., Mejia, A., Cobian, M., Becker, T., & Nicolaidis, C. (2014). Latino Parents’ Perspectives on Barriers to autism diagnosis. Academic Pediatrics, 14(3), 301–308. https://doi.org/10.1016/j.acap.2013.12.004